Table of Contents

Autoimmune disorders are conditions in which our immune system, which is responsible for safeguarding our body against invaders, mistakenly targets its cells, tissues and organs. This misdirected and overactive immune system response can result in inflammation and harm to parts of the body. Different symptoms of disorders are varied. Can impact multiple systems. Common indications include exhaustion, discomfort and swelling in the joints swollen glands. Skin issues like rashes, muscle ache, weakness and hair loss may also be experienced.
What triggers autoimmune diseases?
Moreover autoimmune disorders can manifest as problems like neurological symptoms, recurring fevers, sensitivity to light and mouth sores. It’s important to emphasize that common symptoms of autoimmune disease can greatly differ from person to person and it is vital to consult a healthcare professional for a diagnosis.
Research Shows Biomedical Discoveries Underpin Good Health
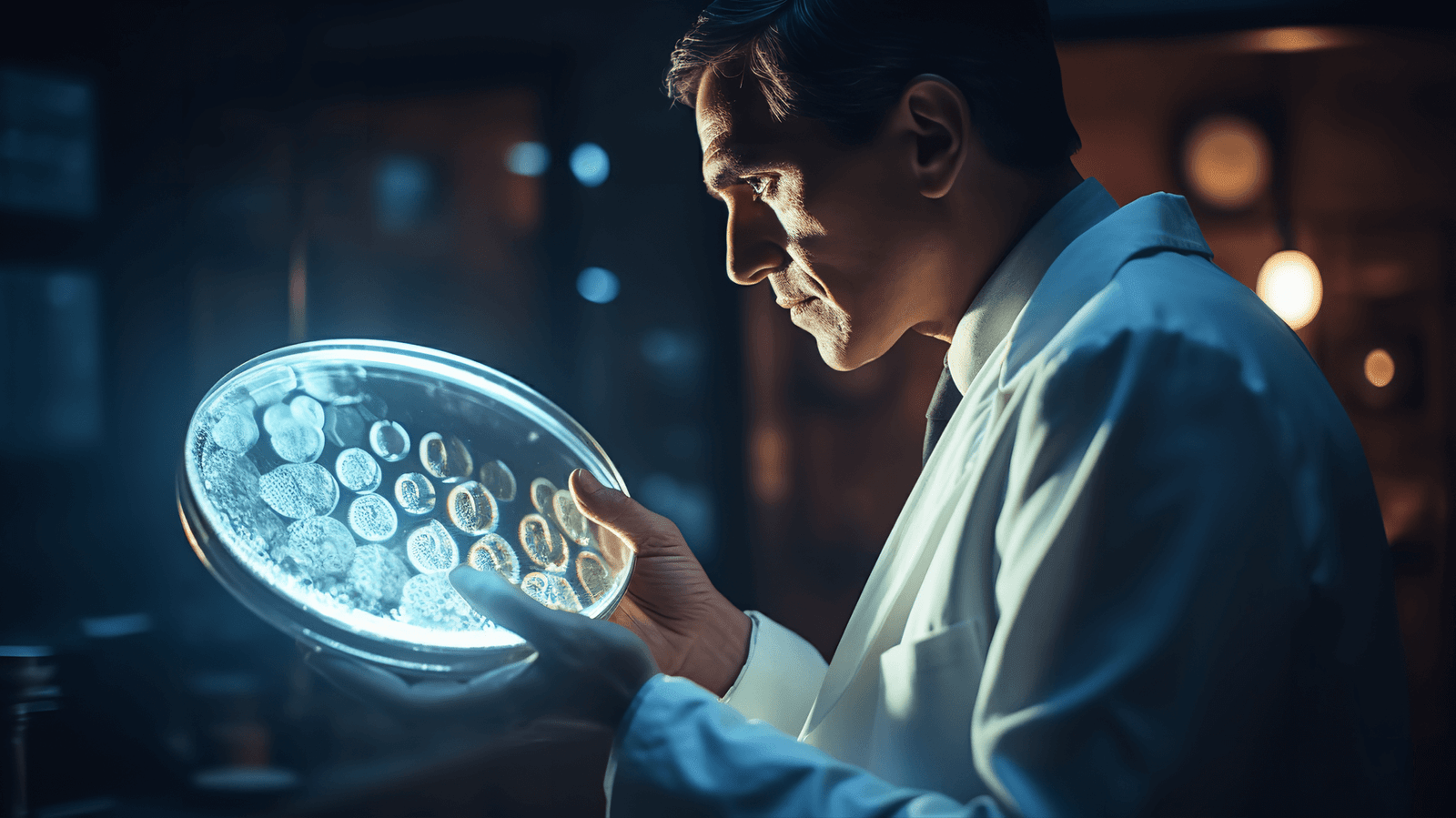
In the last five hundred or so years, almost all medical breakthroughs had been made by forensic scientists unravelling another mysterious molecule. Johns Hopkins’research has produced vaccines, treatments and diagnostic breakthroughs. The Hopkins Institute of Basic Biomedical Science continues its legacy through leading studies of the causes of a wide range of medical conditions.
Autoimmune Disease: Why Is My Immune System Attacking Itself?

The exact cause of disorders with autoimmune antibodies is not fully understood, however, it is likely a combination of genetic, environmental and hormonal factors that play a role. Here are some important factors that contribute to the immune system attacking or mistakenly attacking the red blood cells and bodys tissues:
Genetic predisposition: Autoimmune disorders often have a component. Certain genes can make individuals more susceptible to developing these conditions. However, having a predisposition does not necessarily mean that an individual will definitely develop a disorder.
Environmental triggers: Various environmental factors like infections, exposure to toxins, and other external stimuli can trigger or worsen responses in individuals who are genetically prone to such conditions.
Influences: Autoimmune disorders tend to be more prevalent in women compared to men, suggesting an influence of hormones, potentially changes in hormone levels during puberty, pregnancy and menopause can impact the system.
Immune system dysregulation: In our system there is a delicate balance between defending against harmful invaders and avoiding attacks, on the bodys own cells by mistake.
Cross reactivity is another factor that can contribute to autoimmunity. Sometimes, the body’s immune system attacks itself, mistakenly identifies a part of the bodys tissues as an invader. This confusion can arise when the immune system damages those certain proteins in healthy cells or tissue of the body. As a result, the immune system launches an attack against both the intruder and the bodys own tissues.
Ongoing research in this field aims to gain an understanding of what causes these diseases, and certain factors which may ultimately lead to strategies for prevention and treatment. If you suspect you might have a disease, it is crucial to seek guidance from a healthcare provider who can conduct a thorough evaluation and provide an accurate diagnosis.
Autoimmune Disease Risk Factors
Researchers are still studying what causes autoimmune disorders and some studies show the presence of the immune system in blood cells in the body following an infection cardiovascular disease. Some factors increase our chances for developing autoimmune diseases, notably:
Genetic Inclination:
Inherited Susceptibility: Genetic elements play a significant role in autoimmune diseases. People with a family history of conditions are more likely to have a predisposition. Certain genes associated with immune system regulation and function, can increase susceptibility. However, it’s important to note that having an inclination does not necessarily mean an individual will develop an autoimmune disease; other factors usually come into play.
Gender:
Prevalence in Females: Many autoimmune diseases tend to affect women’s health. Although the exact reasons for this gender bias are not fully understood, it is believed that hormonal influences such as estrogen may contribute to this disparity.
Environmental Triggers:
Infections:Exposure to infections can trigger responses. Molecular mimicry is a phenomenon where the bodys immune system may mistakenly target looking structures, in the body after fighting off an infection leading to autoimmunity. For instance in some cases of fever a complication of infection of autoimmune reactions affecting the heart can occur.
What is the root cause of autoimmune disease?

Hormones play a role in regulating the system by also influencing the development and progression of certain antibodies of autoimmune diseases. Women are more prone to these health conditions and hormonal fluctuations during stages of life. For instance, there is an increased risk in certain risk factors of autoimmune thyroid disorders during the postpartum period.
Autoimmune diseases can occur at any age. Rheumatoid arthritis often starts in older age, while the disease systemic lupus erythematosus (SLE) is more common in women who’re of childbearing age. However, it’s worth noting that children and adolescents can also be affected by diseases.
Different racial and ethnic groups may have variations in genetic factors in the prevalence of diseases. For example, systemic lupus erythematosus is commonly found among American and Hispanic populations.
It’s crucial to understand that autoimmune diseases encompass a range of conditions, each with its health history and its unique set of risk factors and complexities.
Autoimmune Disease and Your Health
Living with an autoimmune disease may require continuous adjustments, as the experience can differ greatly among individuals. It’s important to regularly communicate with healthcare professionals, have a strong support system and take a proactive approach to self care in order to effectively manage life with an an autoimmune disorder. Here are some important aspects to consider when navigating life with an autoimmune disease:
Regular Medical Check ups: Consistently monitoring your health is crucial for tracking the progression of the autoimmune disease, managing symptoms and adjusting treatment plans as necessary.
Medication Adherence: It’s essential to follow prescribed medication regimens in order to control symptoms and prevent flare ups.
Balanced Diet: A well balanced and nutritious diet can contribute to overall health and may have specific benefits for managing autoimmune conditions. Some individuals find relief from symptoms by adopting anti inflammatory diets.
Adequate Rest: Fatigue is a common symptom of autoimmune diseases. Ensuring you get sufficient rest and practicing good sleep is essential for managing energy levels and overall health.
Ways to Reduce Stress: Dealing with chronic stress can make autoimmune symptoms worse. Incorporating techniques like meditation, yoga, deep breathing or mindfulness into your routine can contribute to your overall well being.
Seeking Counseling: Living with a chronic condition can have an emotional toll. Professional counseling or joining support groups can provide a safe space to express feelings, address fears and navigate the challenges that come with autoimmune diseases.
Adjusting Work and Daily Activities: Depending on the severity of your symptoms, you may need to make modifications to your work schedule or daily routines. This could involve adapting your workspace or utilizing assistive devices.
Understanding Rights and Resources: Advocating for yourself means being aware of your legal rights, workplace accommodations, as well as available resources.
Maintaining Open Communication with Healthcare Providers: Establishing a transparent line of communication with healthcare providers encourages a collaborative approach to effectively managing the autoimmune disease.
While taking steps to reduce cardiovascular disease like blood pressure medications can always work out well for some people, it can also be beneficial for you. Keep the blood pressure in arteries in check, eating the right diet and consuming enough exercise daily are all vital for the body. This can help reduce autoimmune symptoms. Often the organ function of the immune system is restricted by autoimmune arthritis and a medication that suppresses it can reduce kidney damage and its effectiveness by inhibiting its immune system.
Autoimmune diseases: What are other common autoimmune diseases?

Some common autoimmune diseases are:
Lupus: Lupus, also known as lupus erythematosus (SLE), is an autoimmune condition that can impact various organs and systems within the body. From protecting the body from invaders, like bacteria and viruses, the immune system in lupus becomes overactive and mistakenly attacks its own tissues and organs, causing tissue damage. This dysfunction in the immune system attacks and can lead to inflammation and damage in parts of the body. While the exact cause of why lupus occurs is not completely understood, it is believed to involve a combination of environmental and hormonal factors that help develop the lupus symptoms. Diagnosis systemic lupus usually involves assessing symptoms conducting blood tests and other laboratory evaluations.
What is the life expectancy of a person with Lupus?
Although lupus does not have an influence, on life expectancy it is important to note that complications arising from the disease can have an impact on health outcomes. One major concern associated with lupus is the potential, for organ damage specifically affecting the kidneys and cardiovascular central nervous system together. Such damage can significantly influence the prognosis of individuals affected by lupus.The focus of treating lupus typically revolves around managing symptoms preventing flare ups and minimizing harm to organs. Doctors may prescribe certain medications, such as inflammatory drugs, corticosteroids or immunosuppressants as part of the treatment plan. Additionally making lifestyle adjustments to relieve symptoms, like practicing sun protection measures and stress management techniques are aspects of managing lupus.
Multiple sclerosis: Multiple sclerosis (MS) is a term condition that affects the central nervous system (CNS) which encompasses the brain and spinal cord. In individuals, with MS the body’s immune system attacks or mistakenly targets the covering of nerve fibers known as myelin causing inflammation and damage. This damage disrupts the transmission of signals along the nerves resulting in a wide array of symptoms. Living with MS requires attention, support and adaptation to evolving symptoms as individuals with MS often collaborate closely with healthcare professionals, such as neurologists and other specialists, to develop treatment plans that cater to their needs and challenges. Timely diagnosis and intervention can assist in managing the impact of the disease and enhancing long term outcomes.
Eczema and Psoriasis: Eczema and psoriasis are two types of long term skin conditions that can lead to discomfort and impact the way your skin looks. Although they have their differences it can sometimes be difficult to tell them. To get a diagnosis and suitable treatment for health conditions it’s best to consult a healthcare professional, a dermatologist, who can assess the unique characteristics of your skin condition.
Thyroid Hormone: The thyroid hormone is a gland shaped like a butterfly, can be swollen glands found in the throat, developing something called butterfly rash. Its role is vital in regulating processes and supporting the hormones produced by the thyroid to have an impact on metabolism, energy production as the functioning of organs and tissues. The development of autoimmune disease and thyroid diseases is influenced by a combination of factors like genetics, environment and hormones, genetics can make an individual more susceptible while environmental factors like infections, stress and exposure, to substances may either trigger autoimmune disease or worsen reactions.
Astma: Asthma is a term condition marked by inflammation and narrowing of the airways causing difficulties, in breathing. It’s an ailment that can impact people of all ages although it often begins during childhood. Asthma typically exhibits recurring episodes of wheezing, shortness of breath chest tightness and coughing. The intensity and frequency of these symptoms can differ from person to person.
Celiac Disease: Celiac disease is a condition that affects the intestine and is caused by consuming gluten, normally found in food. Gluten is a protein found in wheat, barley, rye and their related products. When people, with disease eat gluten it triggers a response that harms the lining of the small intestine. This damage hinders nutrient absorption. Can cause a range of symptoms and potential long term health issues. It’s important to note that celiac disease can impact organs and systems beyond the digestive tract. Some possible long term complications include deficiencies, weakened bones (osteoporosis) difficulties getting infertility) as well as an increased risk, or higher risk of, for certain symptoms of autoimmune, disorders and cancers.
Rheumatoid Arthritis: Rheumatoid arthritis (RA) is a lasting immune system condition that primarily targets the joints in our bodies. In RA the bodys defenses mistakenly attack the synovium, which’s the lining, around the joints. This immune response leads to inflammation in the affected joints resulting in the joint pain and, swelling, stiffness and eventually joint damage.
When should I see my healthcare provider?
Consult the physician when the condition changes. Even small changes to certain medications in your experience are important. Talk to your doctor if you feel that your medications can’t treat Lupus. Tell a healthcare provider if you are experiencing a flare-up more frequently. The doctor will assist in the appropriate adjustments of treatment. You can go to an emergency medical facility, emergency department, 911, emergency service, 911, or 911.
Symptoms of Systemic Lupus Erythematosus (Lupus)

It can affect people with severe lupus symptoms as well as mild lupus occurs. You may only have symptoms affecting the body’s most basic organs, but you may have multiple symptoms. Lupus symptoms may arise and change, causing recurring pain or a developing symptom that will trigger lupus. It may cause inflammatory diseases in organs such as joints, skin cells, kidneys, heart lining and lungs because lupus affects many parts of healthy tissue in the body. It can cause inflammatory symptoms throughout the body and cause organ damage such as:
Fatigue: Persistent and overwhelming tiredness is a symptom experienced by individuals, with lupus. It can have an impact on activities and overall quality of life.
Joint Pain and Swelling: Lupus often leads to pain and swelling that resembles similar symptoms seen in arthritis. The involvement of joints can be symmetrical.
Skin Rash: A unique butterfly shaped rash on the face spanning across the cheeks and nose is a characteristic of lupus. Additionally rashes on parts of the body sensitivity to sunlight (photosensitivity) and the presence of skin lesions may also occur.
Fever: Recurrent fevers without a cause are frequently observed in individuals with lupus. Fever developing lupus can be an indication of inflammation or an immune system response.
Muscle Pain: Individuals with lupus may experience muscle pain and muscle weakness which often mimic symptoms associated with myositis, physical therapy must be integrated.
Raynauds Phenomenon: Raynauds phenomenon causes fingers and toes to turn white or blue due to restricted blood flow in response to temperatures or stress.
Kidney Involvement: Lupus nephritis is a complication that occurs when the immune system attacks the kidneys potentially leading to a kidney failure or kidney damage.
Chest Pain: The heart and lungs can be affected by lupus resulting in chest pain inflammation, around the heart (pericarditis) or inflammation of the lungs (pleuritis).
Neurological signs: These may manifest as headaches, seizures, difficulties with thinking and in cases psychiatric symptoms.
Mouth or nasal sores: Some individuals with lupus may experience ulcers in their mouth or nose.
Hair thinning: Losing hair in a pattern is a common indication of lupus.
Sensitivity to sunlight: Increased sensitivity to sunlight that can result in skin rashes or flare ups and skin problems when exposed to the same sun exposure amount.
Gastrointestinal problems: Lupus can lead to issues such as nausea, vomiting and other abdominal pain and discomfort.
Blood disorders: Anemia, low platelet count (thrombocytopenia) and abnormalities in red blood cells) may occur in individuals, with lupus.













Discussion about this post